The patient education process is a clear, structured approach that helps patients understand their health, take part in care decisions, and adopt behaviors that improve outcomes. Today, effective patient education is essential—it is a core part of clinical and operational care.
Moreover, healthcare organizations increasingly rely on digital patient education solutions to deliver consistent, measurable education at scale. These solutions support safety, engagement, and compliance while improving the overall patient experience
What Is the Patient Education Process?
The patient education process is a continuous, patient-centered cycle designed to help individuals acquire the knowledge, skills, and confidence needed to manage their health effectively. Unlike traditional information delivery, this process focuses on understanding, behavior change, and self-management.
Research-based guidelines define patient education as a collaborative process that adapts to:
- Patient literacy and numeracy levels
- Language and cultural background
- Emotional readiness and motivation
Low health literacy and numeracy are well-documented barriers to safe care, which is why structured education is essential
Core Principles of an Effective Patient Education Process
An effective patient education process is built on several key principles that guide all education activities:
- Patient-centered and individualized
- Behavior-focused rather than solely information-based
- Delivered using plain language
- Reinforced through interaction and repetition
- Evaluated using measurable outcomes
These principles align with international best practices and support safer transitions of care and better long-term outcomes.
The 4-Step Patient Education Process Explained

The steps of patient education process is widely adopted across hospitals, clinics, and healthcare systems. Each step is essential and should not be skipped.
1. Assessment
Assessment identifies what the patient needs, values, and can realistically do.
Key assessment elements include:
- Current understanding of the condition
- Health literacy and numeracy level
- Preferred learning format (verbal, written, visual, digital)
- Language and cultural considerations
- Barriers such as anxiety, pain, or limited support
Without proper assessment, patient education risks being generic, ineffective, and unsafe.
2. Planning
Planning transforms assessment findings into a structured education plan developed with the patient, not just for the patient.
Effective planning includes:
- Defining clear, measurable learning goals
- Prioritizing behaviors critical to safety and self-care
- Selecting appropriate education tools and formats
- Coordinating education across the care team
Healthcare organizations often integrate this step into broader patient experience and quality improvement initiatives
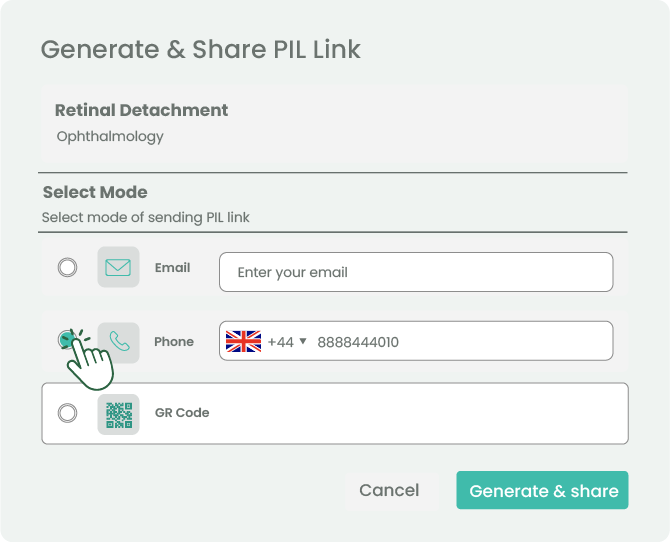
3. Implementation
Implementation is the delivery of education using evidence-based strategies that promote understanding and retention.
Best practices include:
- Using plain, non-medical language
- Teaching in short segments (“chunk and check”)
- Applying teach-back techniques
- Combining verbal, written, and visual materials
- Encouraging questions and dialogue
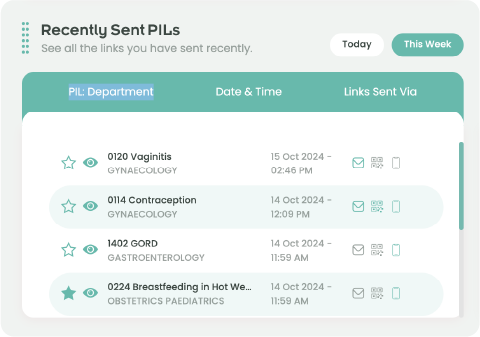
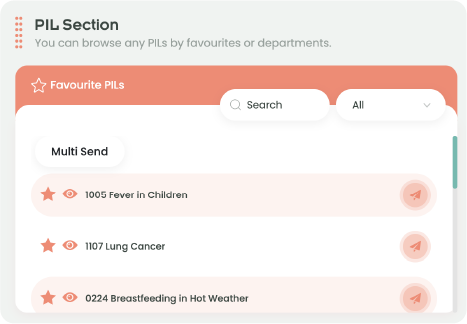
Digital platforms help standardize implementation while maintaining personalization, especially in busy clinical environments.
4. Evaluation
Evaluation confirms whether education was effective and whether the patient can apply what they learned.
Common methods include:
- Teach-back to verify understanding
- Return demonstration of skills
- Monitoring adherence and outcomes
- Identifying the need for reinforcement or re-teaching
As a result, evaluation closes the loop and ensures patient education contributes to real-world outcomes.
What Are the Goals of the Patient Education Process?
Understanding what are the goals of the patient education process helps organizations align education with clinical, operational, and business priorities.
Key goals include:
- Improving patient confidence and self-management
- Supporting safe adherence to treatment plans
- Reducing avoidable errors and readmissions
- Enhancing communication and trust
- Improving measurable quality and safety indicators
These goals directly support value-based care models and long-term patient engagement.
Why the Patient Education Process Is important for Healthcare Providers
A standardized patient education process benefits healthcare organizations by:
- Supporting accreditation and compliance
- Reducing variation in patient instructions
- Improving continuity of care
- Strengthening patient trust and satisfaction
- Enhancing quality and safety metrics
Moreover, when combined with digital patient education tools, organizations can scale education efficiently while maintaining quality and consistency.
Conclusion
A structured patient education process enables healthcare organizations to deliver consistent, patient-centered education that drives safer behaviors and better outcomes. By applying a clear, step-based approach and supporting it with the right tools, organizations can improve care quality, engagement, and operational efficiency.
FAQs About the Patient Education Process
How does the patient education process impact organizational risk and liability?
Clear, documented patient education reduces misunderstandings, supports informed consent, and lowers the risk of adverse events related to improper self-care or non-adherence.
Can the patient education process be integrated into EMR or HIS systems?
Yes. Many healthcare organizations integrate patient education content into EMR systems to automate delivery, track completion, and document education as part of the clinical workflow.
How often should patient education materials be reviewed or updated?
Education materials should be reviewed regularly to reflect updated clinical guidelines, regulatory requirements, and patient feedback, ensuring accuracy and relevance over time.
What KPIs can be used to measure the success of the patient education process?
Common indicators include patient engagement rates, comprehension scores, adherence metrics, reduction in avoidable readmissions, and patient-reported experience measures.
Is patient education cost-effective for healthcare organizations?
Yes. A standardized patient education process reduces repeated explanations, prevents complications, improves adherence, and ultimately lowers avoidable healthcare costs.
How does patient education support population health initiatives?
Patient education plays a critical role in population health by promoting preventive behaviors, improving chronic disease self-management, and supporting long-term community health outcomes.
References
Health Care Education Association – Patient Education Guidelines.
Armstrong, M. L. (1989). Orchestrating the process of patient education. Nursing Clinics of North America, 24(3), 597–604. link