Patient education is vital for improving health literacy and adherence. Despite its importance, healthcare professionals face multiple barriers to patient education that limit understanding and outcomes.
To provide the best care, healthcare professionals must recognize these obstacles and address them with consistent, inclusive strategies.
Understanding the Importance of Patient Education
Effective patient education strengthens relationships between healthcare providers and patients. It also improves compliance, satisfaction, and long-term health outcomes across all care settings.
Moreover,When patients understand their diagnoses and treatment plans, they manage chronic diseases better and take an active role in prevention.
On the other hand, If patients misunderstand information or miss proper education, they and the healthcare system face avoidable physical, emotional, and financial consequences.
Studies show literacy levels, culture, and system barriers remain central challenges to effective education delivery.
Common Barriers to Patient Education
Several factors sustain barriers to patient education; therefore, coordinated strategies are needed to improve understanding, communication, and knowledge retention.
1. Patient-Related Barriers
- Low health literacy: Many patients struggle to read or interpret medical instructions, particularly those with limited formal education.
- Cultural and language differences: Misunderstandings arise when healthcare providers do not adapt their patient education materials or verbal communication to the patient’s cultural context.
- Emotional and physical states: Pain, anxiety, fatigue, or fear of diagnosis may interfere with learning and retention.
- Lack of motivation: Some patients may not see the value of the information, especially when their symptoms feel mild or manageable.
2. Nurse-Related and Provider Barriers
- Time constraints: High patient loads and administrative duties reduce opportunities for individualized education.
- Insufficient training: Some nurses report limited preparation in communication techniques or adult learning principles.
- Attitudinal issues: A lack of confidence in teaching ability or assumptions about patient interest can reduce the effort invested in education.
- Language and cultural mismatches: Providers who do not share linguistic or cultural backgrounds with their patients may inadvertently overlook key learning cues.
Consequently, these barriers to patient education in nursing are among the most frequently cited in literature and can significantly impact patient adherence and satisfaction.
3. Systemic and Environmental Barriers
- Limited educational materials: Outdated or overly technical resources make comprehension difficult.
- Poor infrastructure: Noisy wards, lack of privacy, and time-limited consultations disrupt the learning process.
- Inadequate policies: When patient education is not institutionalized as part of routine care, it often becomes an afterthought.
- Technology gaps: Not all patients have access to digital tools used in modern education programs, such as patient portals or online learning platforms.
Barriers to Health Education Across Settings
In hospitals, health education is often affected by workflow pressure, meanwhile, community and outpatient settings also present challenges, including misinformation and socioeconomic inequalities.
Socioeconomic status, unreliable online information, and cultural health beliefs can cause misunderstanding, mistrust, or resistance toward evidence-based medical advice and guidance.
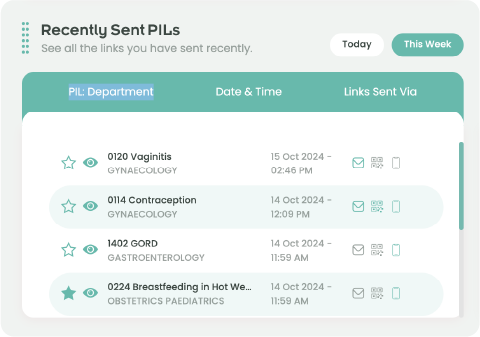
Furthermore, primary care providers and pharmacists frequently struggle to ensure continuity of education once patients leave clinical environments, creating gaps in understanding and compliance.
In resource-limited areas, these challenges intensify due to lack of trained educators, few materials in local languages, and insufficient policy support for education initiatives.
Overcoming Barriers to Patient Education

Addressing the barriers to patient education requires a collaborative, culturally sensitive, and evidence-based approach.To achieve this, healthcare teams can follow several strategies:
1. Assessing individual learning needs
Evaluate each patient’s literacy level, cultural background, and preferred learning style before delivering information.
2. Using plain language and visual aids
Simplify instructions and reinforce key messages through charts or demonstrations.
3. Allocating dedicated teaching time
Integrate education into care plans, rather than treating it as an optional add-on.
4. Enhancing staff training
Incorporate empathy teaching methodologies and empathy communication skills into ongoing professional development for nurses and physicians.
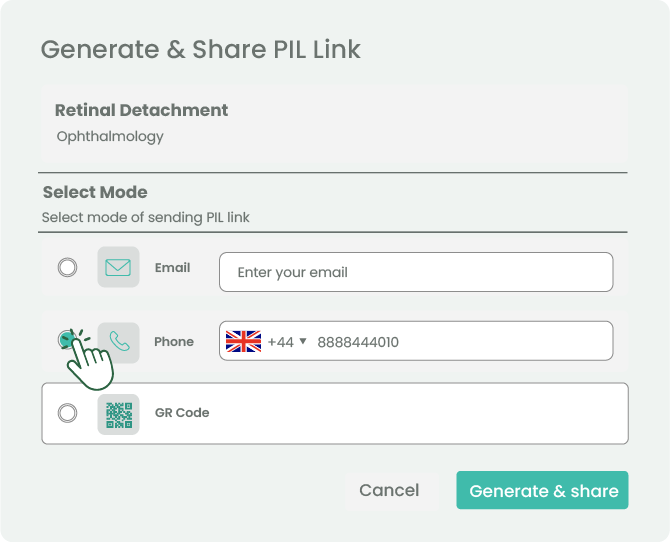
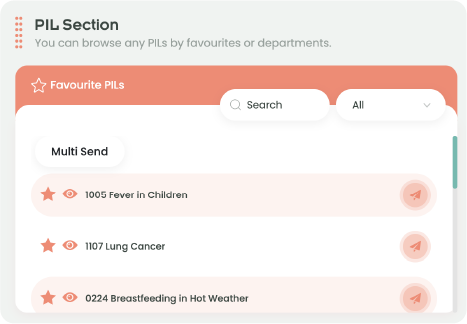
5. Leveraging technology wisely
Use mobile apps, digital videos, and interactive HTMLs to support learning continuity.
6. Promoting interdisciplinary collaboration
Involve pharmacists, dietitians, and educators to provide consistent, patient-centered information.
Conclusion
Overcoming barriers to patient education demands empathy, collaboration, and cultural awareness.
By simplifying information and adapting it to patient needs, healthcare professionals can bridge communication gaps and foster understanding.
Empowering patients through clear, inclusive education improves adherence, builds trust, and strengthens outcomes.
Ultimately, effective patient teaching transforms care delivery, creating a safer, more informed, and patient-centered healthcare system.